Publicado el marzo 25, 2024
Terapia fototerapéutica domiciliaria para el vitiligo
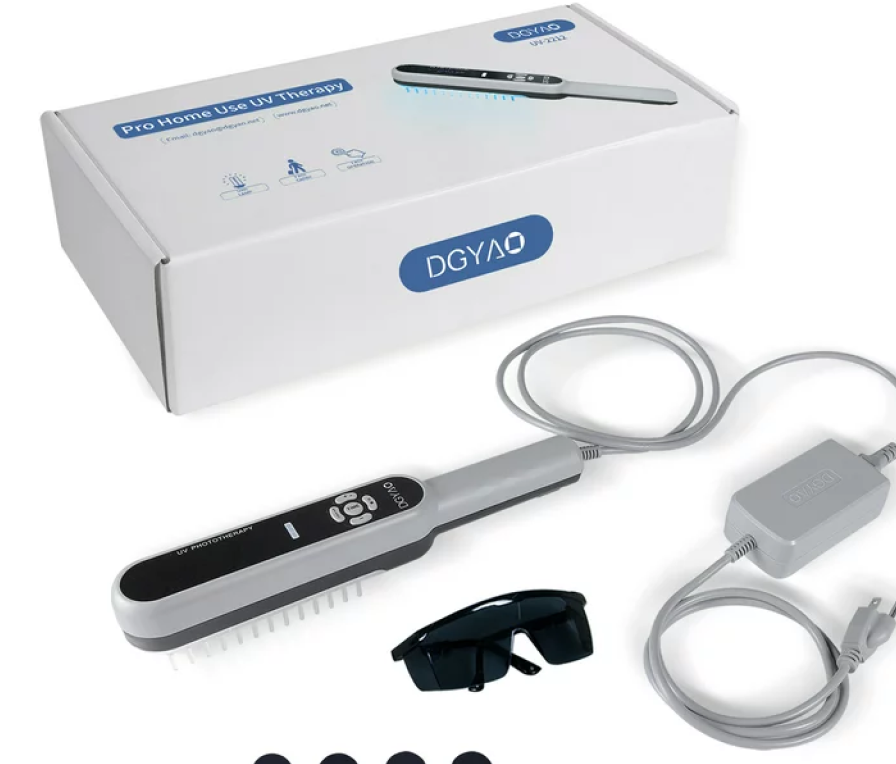
Eleftheriadou y sus colegas (2014) señalaron que las unidades de NB-UVB de mano son dispositivos ligeros que podrían superar la necesidad de tratar el vitiligo en gabinetes de fototerapia en hospitales, permitiendo un tratamiento temprano en casa que podría aumentar la probabilidad de una repigmentación exitosa.
El ensayo piloto Hi-Light examinó la viabilidad de realizar un gran ensayo clínico aleatorizado y controlado (RCT) sobre el uso de tales dispositivos al explorar el reclutamiento, la adherencia, la aceptabilidad y la educación de los pacientes. Este fue un RCT de viabilidad, doble ciego, multicéntrico, en grupos paralelos de fototerapia NB-UVB de mano para el tratamiento del vitiligo en casa. La duración total del ensayo fue de 7 meses; 3 meses de reclutamiento y 4 meses de tratamiento. Los participantes fueron aleatorizados a grupos activos o placebo (relación 2:1).
El principal indicador de resultado fue la proporción de participantes elegibles que estuvieron dispuestos a ser aleatorizados. Los resultados secundarios incluyeron la proporción de participantes que expresaron interés en el ensayo y cumplieron con los criterios de elegibilidad, tasas de abandono y datos faltantes, proporción de participantes que se adhirieron al tratamiento y estuvieron satisfechos con él, y la incidencia de eventos adversos a corto plazo de NB-UVB. Un total del 83 % (45/54) de los pacientes con vitiligo que expresaron interés en el ensayo estuvieron dispuestos a ser aleatorizados.
Debido a limitaciones de tiempo y recursos financieros, solo 29/45 participantes potenciales fueron programados para asistir a una visita inicial en el hospital. Los 29 (100 %) participantes potenciales fueron confirmados como elegibles y posteriormente aleatorizados. La disposición a participar en el estudio para consultas de Medicina General (médicos de familia) y hospitales fue del 40 % y 79 %, respectivamente; el 86 % (25/29) de los pacientes se adhirieron al tratamiento y el 65 % (7/11) de los pacientes en el grupo activo mostraron algún grado de repigmentación. Solo 1 paciente en el grupo activo reportó eritema grado 3 (3 %). Ambos dispositivos (Dermfix 1000 NB-UVB y Waldmann NB-UVB 109) fueron aceptables para los participantes.
Los autores concluyeron que los dispositivos de mano NB-UVB necesitan ser evaluados en un gran ensayo clínico pragmático. Este ensayo piloto ha explorado muchas de las incertidumbres que deben superarse antes de realizar un ensayo a gran escala, incluida la elaboración de un paquete de formación integral y un protocolo de tratamiento. El estudio mostró una fuerte disposición de los participantes a ser aleatorizados, una muy buena adherencia al tratamiento y tasas de repigmentación, y proporcionó evidencia de viabilidad para un ensayo definitivo. Este ensayo no fue diseñado como un ensayo de eficacia.
Ashraf y sus colegas (2022) señalaron que el vitiligo puede ser tratado con fototerapia en hospitales; sin embargo, esto requiere citas frecuentes a largo plazo. El auto-tratamiento utilizando fototerapia en casa es una alternativa conveniente, que podría mejorar la adherencia y los resultados, pero la evidencia es limitada, por lo que no se recomienda rutinariamente. En una revisión sistemática, estos investigadores examinaron la seguridad y efectividad de la fototerapia en casa para el vitiligo.
Realizaron búsquedas en Medline, Scopus y la Cochrane Library de ensayos clínicos aleatorizados (RCTs) que comparaban la fototerapia en casa con la fototerapia institucional o placebo/no fototerapia para el vitiligo. El resultado principal fue la efectividad del tratamiento. Se utilizaron los criterios CASP para la evaluación de la calidad. Los datos fueron sintetizados en un metaanálisis donde fue apropiado.
Un total de 3 estudios (195 sujetos) fueron incluidos: 2 compararon fototerapia en casa con fototerapia institucional, y 1 comparó fototerapia en casa con placebo. Los estudios eran de calidad mixta. Los regímenes de tratamiento variaron entre los estudios. Los hallazgos sobre la efectividad fueron contradictorios entre los estudios con tasas variables de repigmentación. No hubo una diferencia significativa en las tasas de repigmentación entre los 2 grupos, aunque la adherencia a los horarios de tratamiento fue significativamente mejor en los grupos de fototerapia en casa.
Los efectos adversos fueron significativamente más altos en los grupos de fototerapia en casa. No se reportaron datos a largo plazo sobre el mantenimiento de los beneficios del tratamiento. Los autores concluyeron que, aunque la adherencia al tratamiento fue significativamente mejor con la fototerapia en casa, los datos eran insuficientes para sacar conclusiones sobre la efectividad. Estos investigadores afirmaron que la fototerapia en casa tenía un riesgo significativamente mayor de efectos adversos, lo que dificultaba recomendarla en la práctica clínica.
Sin embargo, como ofrecía ventajas logísticas para los pacientes, su efectividad junto con medidas de seguridad adicionales debe ser examinada más a fondo en ensayos clínicos aleatorizados de gran escala y buena calidad, con medidas de resultado estandarizadas, incluyendo los resultados reportados por los pacientes.
Referencias
- https://www.aetna.com/cpb/medical/data/400_499/0422.html
- Eleftheriadou V, Thomas K, Ravenscroft J, et al. Feasibility, double-blind, randomised, placebo-controlled, multi-centre trial of hand-held NB-UVB phototherapy for the treatment of vitiligo at home (HI-Light trial: Home Intervention of Light therapy). Trials. 2014;15:51.
- Ashraf AZ, Azurdia RM, Cohen SN. The effectiveness of home-based phototherapy for vitiligo: A systematic review of randomised controlled trials. Photodermatol Photoimmunol Photomed. 2022;38(5):409-417.