COVERAGE CONSIDERATIONS
Factors That Influence Coverage
Third-party payers (e.g., commercial insurers, Medicare, Medicaid) will generally cover parenteral drugs for their approved U.S. Food and Drug Administration (FDA) indications and the associated professional administration services. However, benefits may vary depending upon the payer and the specific plan (“insurance product”) in which a patient is enrolled.
- Medical Necessity
When third-party payers review claims, they will first determine if the type of service provided is covered under their policies. Next, payers will look for evidence supporting the medical necessity of the therapy. This evidence may include:
- Information about the patient’s medical condition and history
- A physician’s statement or Letter of Medical Necessity
- Supporting literature (e.g., peer-reviewed studies and compendial monographs)
- Full Prescribing Information
- Availability of other treatment alternatives
Medical necessity refers to a decision by a health plan that a treatment, test, or procedure is necessary for health or to treat a diagnosed medical problem. Health insurance companies provide coverage only for health-related services that they define or determine to be medically necessary.
Medicare National Coverage Determinations (NCD) and Medicare Administrative Contractors (MACs) Local Coverage Determinations (LCDs) define medical necessity requirements for Medicare coverage. These documents contain guidance on covered diagnoses, required documentation, and limitations of coverage for specific services in accordance with medical necessity.
2. Administrative Considerations
Other considerations may be involved in a payer’s decision to cover a product or service:
- Does the payer’s contract specifically indicate the sites of care that may bill for infusion services or infused drugs? A small portion of payers have exclusive contracts with designated preferred providers for infusion services. This may include certain clinics or specialty pharmacies that deliver drugs to healthcare providers or other infusion centers.
- Does the payer cover the therapy only when provided through a specific treatment site? Payers may have site-specific coverage rules that restrict provision of infused therapies. For example, currently Medicare does not cover infusions when they are billed by Medicare-certified ambulatory surgery centers. Payers also may restrict coverage for certain infused drugs in the home or hospital outpatient setting.
- Is the billing provider a “participating” member of, or “in-network” provider for, that particular plan? Payers contract with providers to deliver services to the plan’s members. Providers are thus “participating” or within that plan’s network, requiring them to abide by the contract charge structure when providing care for that plan’s members.
- Is the plan willing to grant in-network status when a service is otherwise out of network? In some cases (e.g., when there are no available in-network providers), health plans may grant in-network status for a provider and related services. In such cases, the provider accepts the in-network rate and the patient will be able to access in-network cost-sharing. It may be helpful to contact a payer to ask for a service to be converted to in-network status.
- If required by the plan, has the appropriate referral or prior authorization been obtained? Many plans require that non-emergency services be pre-approved or that a primary care physician makes the referral for specialty care. Failing to obtain appropriate referrals or pre-authorization can result in non-payment by the plan.
SUPPORTING APPROPRIATE PAYER COVERAGE DECISIONS
An essential component of successfully providing drug therapies is working with payers. Most payers will cover medically necessary drug therapies but may require clinical justification beyond a diagnosis to establish the patient’s need and appropriateness for the therapy. Such requirements may be detailed in drug-specific policies, such as a Medicare Administrative Contractor’s (MAC) Local Coverage Determination (LCD) or a commercial payer’s medical benefit policy or addressed through a general prior authorization process.
- Prior Authorization
Prior authorization (PA) is a payer-required approval process used to assure that certain drugs, services, procedures or sites of care are medically necessary and used appropriately. Although not applicable to Original Medicare, PA may be required by Medicare Advantage and non-Medicare payers. During the PA process providers are required to submit evidence of medical necessity which may include:
- the expected outcome of a prescribed therapy,
- potential consequences of not using that therapy, and
- why alternatives are not clinically appropriate.
An adequately supported and appropriately submitted PA will generally result in a favorable coverage decision. If for some reason a patient cannot meet a payer’s requirements for the drug they need, they have the right to request a coverage determination, also known as requesting an exception.
2. Exception Request
An exception request is a specific type of coverage determination that asks a payer to reconsider a coverage denial or to deviate from standard process. It provides the payer an opportunity to influence, or make more patient-specific, a coverage decision-making process when the payer’s coverage policies do not meet a patient’s unique needs. An exception request again requires the prescriber to submit evidence of medical necessity. It is helpful to specifically respond to the reason(s) coverage was denied (e.g., drug not on formulary, dose restrictions, step therapy, etc.). An exception request that is appropriately submitted and adequately supported will often result in a favorable payer decision. If the request is not granted, the payer will provide the patient with a written explanation and include information about how to request an appeal.
3. Appeals
Appeals are a response to a payers’ denial of benefits the enrollee believes they are entitled to receive. The appeals process typically includes a series of progressive steps and specific timelines. If supporting an appeal, contact the payer for guidance as individual policies may vary. Steps patients or providers can take to support an appeal include:
- submitting supporting evidence to counter the specific reason for the denial
- presenting the patient’s story in a manner that leads to the therapeutic request (e.g., events leading to current condition, results of
previous therapies, expected clinical progression, etc.)
- expressing willingness to collaborate (e.g., offer contact information, invite discussion with a medical director or specialist, etc.)
Following a positive coverage decision at any stage, it is important to provide feedback to the payer and reinforce that their decision resulted in a positive patient outcome.
Phototherapy for Skin Conditions
Most companies consider the following interventions medically necessary:
- Narrow-band UVB phototherapy for the following indications:
- Atopic dermatitis (atopic eczema)
- Chronic urticaria
- Cutaneous mastocytosis (after conventional therapies have failed)
- Cutaneous T-cell lymphoma
- Early-stage mycosis fungoides/Sézary syndrome
- Granuloma annulare
- Kyrle disease (perforating dermatosis) that is refractory to topical or intralesional therapy
- Lichen planus
- Morphea (circumscribed scleroderma)
- Photodermatoses (e.g., actinic dermatitis and solar urticaria)
- Pityriasis lichenoides chronica
- Polymorphous light eruption
- Psoriasis
- Prurigo nodularis that is refractory to topical or intralesional corticosteroids
- Uremic pruritus that is refractory to emollients, topical analgesics and oral antihistamines or gabapentin
- Vitiligo
2. UVB with the addition of topical coal tar (also known as the Goeckerman regimen) for persons with severe psoriasis (defined as psoriasis that affects more than 10 % of body surface area);
3. Home phototherapy (UVB) treatment:
- As DME for persons with severe psoriasis with a history of frequent flares who are unable to attend on-site therapy or those needing to initiate therapy immediately to suppress psoriasis flares
- For persons with atopic dermatitis (eczema) who are unable to attend on-site therapy;
4. Home ultraviolet light booths or ultraviolet lamps, as well as replacement bulbs sold by prescription only, for persons eligible for home UVB phototherapy.
The following interventions are considered experimental and investigational because the effectiveness of these approaches has not been established:
- Narrow-band UVB phototherapy for all indications other than those listed as medically necessary above, including:
- Alopecia mucinosa
- Chemical dermatitis/contact dermatitis
- Cholestasis of pregnancy
- COVID-19
- Dermatographic urticaria (also known as dermographism and dermatographism)
- Drug-related hypersensitivity reaction
- Erythema annulare centrifugum
- Erythematous hyper-pigmented macules/papules
- Graft-versus-host disease
- Grover’s disease (transient and persistent acantholytic dermatosis)
- Hailey-Hailey disease
- Hidradenitis suppurativa
- Hypersensitive rash
- Lichen amyloidosis
- Lichen sclerosus
- Lichen simplex chronicus
- Lichenoid dermatitis
- Lymphomatoid papulosis
- Papular mucinosis
- Papular urticaria
- Progressive macular hypomelanosis
- Pruritus
- Scleroderma
- Skin hypo-pigmentation from scarring
- Superficial mixed-cell dermatitis;
2. UVB with the addition of topical coal tar for all indications other than psoriasis (e.g., pemphigoid, pruritis);
3. The use of petrolatum or emollients before ultraviolet radiation, as the clinical benefits this practice have not been evaluated in well controlled trials;
4. Home phototherapy (UVB) for the treatment of cutaneous T-cell lymphoma (mycosis fungoides and Sezary syndrome), and indications other than psoriasis and atopic dermatitis (eczema);
5. Home PUVA treatment because of insufficient evidence of its safety.
Home Therapy
Home therapy should be limited to UVB and is eligible in the home only when the individual requires UVB treatment at least three (3) times per week. PUVA is not an appropriate choice for home therapy. Oxsoralen is a potent photosensitizing agent that should only be used under controlled conditions and under the supervision of a physician.
Home phototherapy may be considered medically necessary for any ONE of the following diagnoses:
- Severe Psoriasis; or
- Atopic Dermatitis/Severe Eczema; or
- Pruritus of Renal Disease; or
- Lichen Planus; or
- Mycosis Fungoides; or
- Pityriasis Lichenoides; or
- Pruritis of Hepatic Disease
Eligibility for a home therapy device is contingent upon compliance with ALL of the following criteria:
- The individual’s condition must comply with one of the eligible diagnoses listed above; and
- Must have a documented positive response to ultraviolet light; and
- Must be chronic in nature requiring long term maintenance exceeding four (4) months; and
- The device must be ordered by the physician; and
- The device must be approved by the Food and Drug Administration; and
- The device must be appropriate for the body surface/area being treated.
- In addition to meeting the eligibility criteria listed above, payment should be limited to the most appropriate device which adequately meets the needs of the individual. All requests for ultraviolet light cabinets and hand-held units will be reviewed on an individual basis
Ultraviolet light therapy and home therapy not meeting the criteria as outlined in this policy is considered not medically necessary.
HCPCS codes for Phototherapy:
E0691 – ultraviolet light therapy system, includes bulbs/lamps, timer and eye protection; treatment area 2 square feet or less as maintained by CMS falls under ultraviolet light therapy systems.
E1399 – durable medical equipment, miscellaneous and is currently being used to bill for inexpensive DME subject to the rules of 42 C.F.R. 414.220, other covered DME subject to the rules of 42 C.F.R. 414.229, and replacement parts of DME subject to the rules of 42 C.F.R. 414.210(e).

Laser Treatment for Psoriasis and Other Selected Skin Conditions
Most companies consider the following interventions medically necessary:
- Excimer and pulsed dye laser treatment for persons with mild-to-moderate localized plaque psoriasis affecting 10 % or less of their body area who have failed to adequately respond to 3 or more months of topical treatments, including at least 3 of the following:
- Anthralin;
- Corticosteroids (e.g., betamethasone dipropionate ointment and fluocinonide cream);
- Keratolytic agents (e.g., lactic acid, salicylic acid, and urea);
- Retinoids (e.g., tazarotene);
- Tar preparations; and/or
- Vitamin D derivatives (e.g., calcipotriene);
No more than 13 laser treatments per course and 3 courses per year are generally considered medically necessary. If the person fails to respond to an initial course of laser therapy, as documented by a reduction in Psoriasis Area and Severity Index (PASI) score or other objective response measurement, additional courses are not considered medically necessary.
2. The use of laser in acne keloidalis nuchae (AKN) for the following indications:
- Laser excision for treatment of extensive scarring observed in plaque or tumor stage acne keloidalis nuchae (AKN), or
- Laser depilation (laser hair removal) for active AKN that is poorly responsive to medical therapy (e.g., oral and topical antibiotics, and intralesional steroids);
Most companies consider considers the following interventions experimental and investigational because of insufficient evidence in the peer-reviewed literature and the effectiveness of these approaches has not been established:
- Combinational use of pulsed dye laser and ultra-violet B (UVB) for the treatment of persons with localized plaque psoriasis;
- The excimer laser or pulsed dye laser in the treatment of forms of psoriasis other than plaque psoriasis;
- Laser treatment for the following indications (not an all-inclusive list):
- Atopic dermatitis
- Cutaneous amyloidosis
- Diabetic skin wounds
- Dissecting cellulitis
- Eczematous lesions
- Facial warts (verrucae)
- Granuloma annulare
- Granuloma faciale
- Herpes simplex labialis
- Hidradenitis suppurativa
- Hidrocystomas
- Jessner lymphocytic infiltration of the skin
- Keratosis pilaris
- Lichen sclerosus
- Lupus erythematodes
- Melasma
- Morphea (scleroderma of the skin)
- Mycosis fungoides
- Necrobiotic xanthogranuloma
- Onychia
- Onychomycosis
- Prurigo nodularis
- Reticular erythematous mucinosis
- Sarcoidosis
- Spongiotic dermatitis
- Vulval intraepithelial neoplasia
- Vulvar inflammatory skin conditions.
- Ablative laser treatment (non-contact, full-field and fractional ablation) for wound healing.
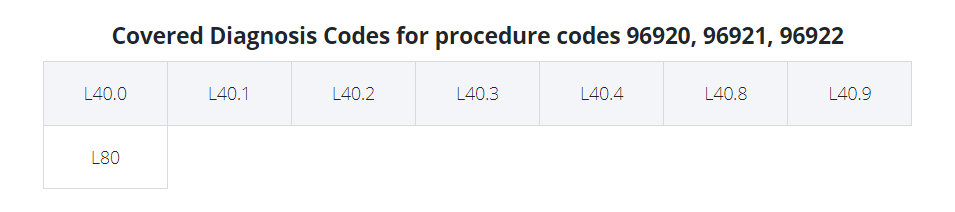
CPT Codes for Laser Treatment
- 96920 Laser treatment for inflammatory skin disease (psoriasis, atopic dermatitis, eczema) total area less than 250 sq cm
- 96921 Laser treatment for inflammatory skin disease psoriasis, atopic dermatitis, eczema) 250 sq cm to 500 sq cm
- 96922 Laser treatment for inflammatory skin disease psoriasis, atopic dermatitis, eczema) over 500 sq cm
These codes technically work only for psoriasis. Some payers will let you use it for other diagnoses (atopic dermatitis, eczema) since there is no other excimer code. If they won’t allow it, you have to use 96999 with a written description attached.
HCPCS Codes (Home phototherapy (UVB treatment):
- A4633 Replacement bulb/lamp for ultraviolet light therapy system, each
Vitiligo
Most companies consider the following established methods medically necessary for the treatment of vitiligo:
- Excimer laser (e.g., XTRAC, PhotoMedex, Radnor, PA; EX-308, Ra Medical Systems, Inc., Carlsbad, CA)
- Narrow-band ultraviolet B (NB-UVB)
- Topical and oral psoralen photochemotherapy (PUVA)
- Topical tacrolimus
- Topical and systemic corticosteroids.
Most companies consider continued PUVA or narrow-band UVB therapy not medically necessary unless there is significant follicular pigmentation after 6 months of therapy (8 to 10 treatments per month).
Most companies consider the following procedures experimental and investigational because the effectiveness of these approaches has not been established:
- The following interventions for the treatment of vitiligo (not an all-inclusive list):
- Apremilast (alone or combined with NB-UVB)
- Autologous mini-punching grafting
- Blister roof grafting (suction epidermal blister grafting) (e.g., CelluTome Epidermal Harvesting System)
- Capecitabine
- Carbon dioxide fractional laser
- Chimeric monoclonal antibody to CD20 (e.g., rituximab)
- Fire needle therapy
- Glutathione
- Home phototherapy
- Interleukins
- Intradermal mesotherapy (injections of bio-revitalizant NCTF135)
- Melagenine
- α-melanocyte stimulating hormone (e.g., afamelanotide)
- Melanocyte transplantation/cultured and non-cultured cellular melanocyte keratinocyte transfer
- Neovir (an intramuscular immunomodulatory agent, composed of sodium oxodihydroacridinylacetate)
- Prostaglandins (e.g., bimatoprost, latanoprost, and prostaglandin E2)
- Split thickness skin grafting
- Tars
- Topical minoxidil
- Topical phenytoin gel
- Topical pseudocatalase
- Tumor necrosis factor-alpha agents (e.g., adalimumab, etanercept, and infliximab)
- Vitamin D analogs (e.g., calcitriol and paricalcitol).
Most companies consider consider treatments for vitiligo cosmetic if they do not affect the underlying condition and do not result in improved protection against skin cancer; specifically micropigmentation (tattooing) and depigmentation (with monobenzylether of hydroquinone/monobenzone) are considered cosmetic.
Resources:
1. https://www.aetna.com/cpb/medical/data/200_299/0205.html