Seborrheic Keratosis and Actinic Keratosis
Actinic keratosis and seborrheic keratosis are two skin conditions that often show up around middle age. Since actinic keratosis lesions can become cancerous, it’s best to get prompt treatment
Actinic Keratosis
Actinic keratosis is a common skin condition characterized by rough, scaly patches on the skin, resulting from prolonged exposure to the sun’s ultraviolet (UV) rays. It is considered a precancerous lesion, meaning it can potentially develop into skin cancer if left untreated. These lesions primarily occur in areas that receive a lot of sun exposure, such as the face, ears, neck, scalp, and hands.
Signs and Symptoms
Actinic keratosis typically presents as small, dry, or rough patches, often resembling sandpaper. These lesions can be tan, pink, red, or even skin-colored and are usually more easily felt than seen. The patches may be itchy or cause a burning sensation in some individuals. Over time, they may thicken or become hard.
Causes
The primary cause of actinic keratosis is long-term sun exposure, which leads to damage in the skin cells. The risk of developing these lesions increases with age and cumulative sun exposure. Individuals with fair skin, light hair, and light-colored eyes are at a higher risk, as their skin is more susceptible to sun damage.
Treatment Options
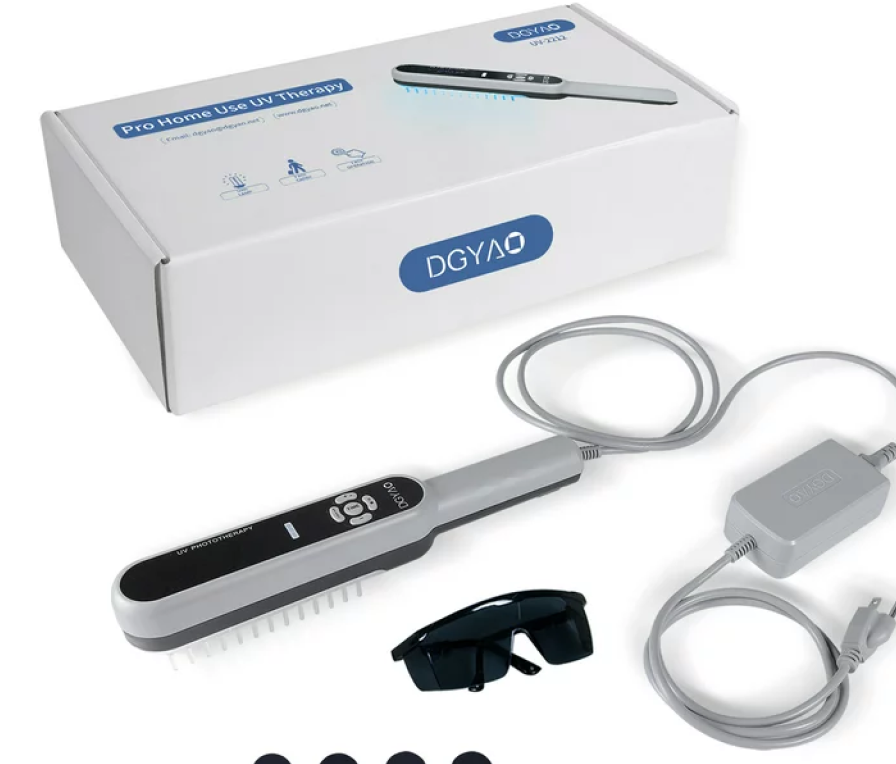
Treatment for actinic keratosis aims to remove or destroy the damaged cells. Options include cryotherapy, where the lesions are frozen off using liquid nitrogen, as well as topical medications such as creams or gels that promote peeling of the damaged cells. In some cases, photodynamic therapy, involving the application of a light-sensitive solution followed by exposure to a special light, may be used. Surgical procedures like curettage or laser treatments are also options, depending on the extent and location of the lesions.
Seborrheic Keratosis
Seborrheic keratosis is another common skin condition, often confused with actinic keratosis due to its appearance. However, it is a benign, non-cancerous growth that typically occurs in older adults and has no risk of developing into skin cancer. Seborrheic keratoses can be found anywhere on the body except on the palms and soles.
Signs and Symptoms
Seborrheic keratosis lesions appear as raised, wart-like growths, ranging in color from light tan to black. They can vary in size from small to over an inch in diameter and often have a waxy or “pasted-on” appearance. These lesions are generally painless but may become irritated by friction from clothing or jewelry.
Causes
The exact cause of seborrheic keratosis is unknown, but genetic factors seem to play a role, as it tends to run in families. Unlike actinic keratoses, seborrheic keratoses are not related to sun exposure. Changes in severity and number of lesions may occur during hormonal shifts or with aging.
Treatment Options
In most cases, treatment for seborrheic keratosis is not necessary unless the growth becomes irritated or a patient seeks removal for cosmetic reasons. Treatment options include cryotherapy, curettage, and laser ablation. Electrosurgery is another method, using an electrical current to remove the lesion.
When to Consult a Professional
Consult a dermatologist if you notice new or changing skin growths. It’s essential to distinguish between potentially precancerous growths like actinic keratosis and benign ones like seborrheic keratosis. Any sudden growth in size, change in color, or persistent itching or bleeding warrants professional evaluation to rule out skin cancer.
Prevention Tips
Preventing actinic keratosis begins with reducing sun exposure. This includes wearing broad-spectrum sunscreen, seeking shade, wearing hats and protective clothing, and avoiding tanning beds. While seborrheic keratosis cannot be prevented, maintaining good skincare and monitoring any changes can aid in early detection and treatment if necessary.
The Bottom Line
Understanding the differences between seborrheic keratosis and actinic keratosis is crucial for proper skin health management. Regular skin checks and consultations with a healthcare professional ensure that any suspicious lesions are appropriately addressed, allowing for early intervention in potentially precancerous conditions.