Published on February 23, 2024
NB-UVB Phototherapy for the Cutaneous Mastocytosis Treatment
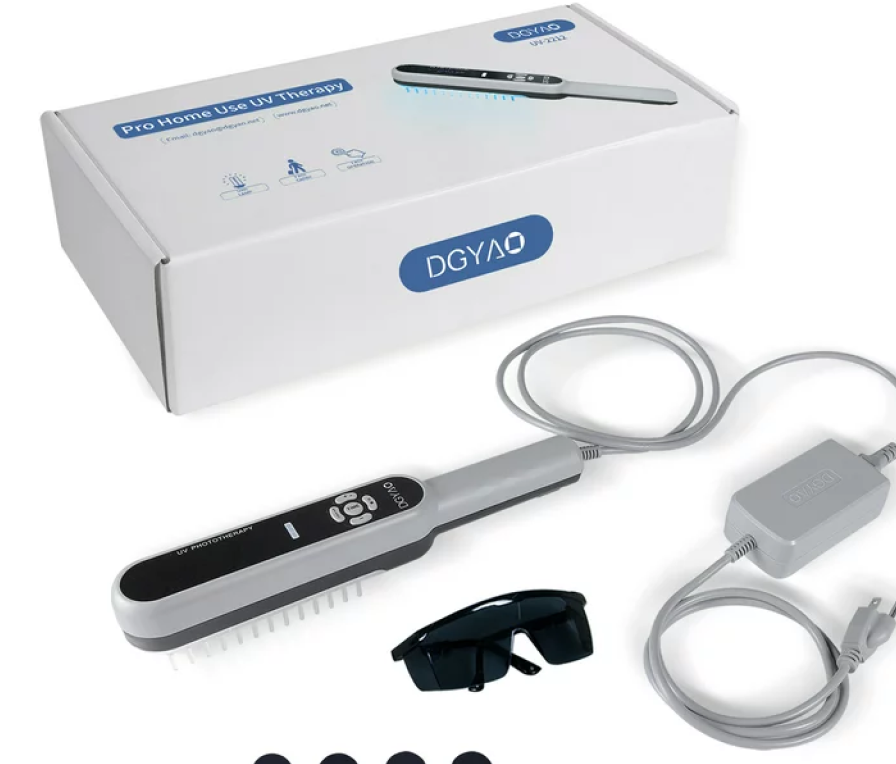
Brazzelli et al (2012) stated that mastocytosis represent a heterogeneous group of stem cell disorders marked by an abnormal hyperplasia and accumulation of mast cells in one or more tissues, including bone marrow, gastro-intestinal (GI) tract, liver, spleen, lymph nodes and skin. Indolent systemic mastocytosis (ISM) is characterized by red-brownish and pruriginous maculopapular lesions, a bone marrow infiltration without functional impairment and an indolent clinical course with a good prognosis. In particular, the most common cutaneous symptoms are urticarial rash and mild-to-high pruritus. These researchers analyzed the clinical outcome of patients affected by ISM with prevalent pruriginous cutaneous symptoms and a scarce response to antihistamines treated using narrowband ultraviolet B (NB-UVB) phototherapy, which was administered in a UV-irradiation cabin equipped with fluorescent UVB lamps with a peak emission at 311 to 313 nm. The perception of pruritus severity was examined using the visual analogue scale (VAS) before starting the treatment and at each control. A complete remission of the cutaneous lesions and pruritus was documented in all patients after a median of 40.3 UV treatments and a median cumulative dose of 51.4 J/cm(2), with a lasting remission over a 6-month follow-up. The median VAS score at the beginning of the treatment was 86.6 (SD = 6.64), whereas it decreased to 6.66 (SD = 3.75) after 3 months of therapy. The authors concluded that the findings of this study provided evidence that NB-UVB phototherapy was useful for the treatment of the cutaneous symptoms and pruritus in ISM.
Brazzelli et al (2016) noted that in mastocytosis, the skin is almost invariably involved, and cutaneous symptoms deeply affect patients’ quality of life (QOL). In a retrospective, observational study, these researchers analyzed the outcomes of patients affected by cutaneous mastocytosis (CM) and ISM treated with phototherapy/photochemotherapy (PUVA or NB-UVB). For each patient, total numbers of PUVA or NB-UVB exposures, the cumulative UV dose (J/cm2 ), serum tryptase profile, and pruritus, before and after treatment, according to the VAS were considered. Skin lesions of each patient were examined, before and after treatment, according to a cutaneous scale score. A total of 20 patients affected by CM and ISM were studied; in particular, 10 patients received NB-UVB therapy, and other 10 patients received PUVA. A statistically significant mean reduction of pruritus in both groups (p < 0.01) was observed. The number of treatments needed to attain symptom relief was significantly lower in the PUVA group, but the mean exposure dose was significantly higher, if compared to the NB-UVB group. Serum tryptase levels showed a downward trend. The cutaneous score improved in both groups. The authors concluded that this study provided evidence that both NB-UVB and PUVA represent a safe and useful 2nd-line therapy of the cutaneous symptoms in mastocytosis. Moreover, these investigators stated that the drawbacks of this trial were that it was a retrospective study with a small sample size (n = 10 in each of the 2 treatment groups) and without a control group.
Furthermore, an UpToDate review on “Cutaneous mastocytosis: Treatment, monitoring, and prognosis” (Castells and Akin, 2020) states that “Psoralen-ultraviolet A therapy (PUVA) or narrow band UVB decreases the number of mast cells and controls pruritus that cannot be managed with antihistamines alone. However, long-term use is associated with an increased risk of skin cancer, and the skin lesions usually recur after therapy is stopped. Phototherapy may be considered for temporary symptomatic relief in patients with diffuse cutaneous mastocytosis with extensive skin involvement refractory to medical management”.
References
- https://www.aetna.com/cpb/medical/data/200_299/0205.html
- Brazzelli V, Grassi S, Merante S, et al. Narrow-band UVB phototherapy and psoralen-ultraviolet A photochemotherapy in the treatment of cutaneous mastocytosis: A study in 20 patients. Photodermatol Photoimmunol Photomed. 2016;32(5-6):238-246.
- Brazzelli V, Grasso V, Manna G. Indolent systemic mastocytosis treated with narrow-band UVB phototherapy: Study of five cases. J Eur Acad Dermatol Venereol. 2012;26(4):465-469.